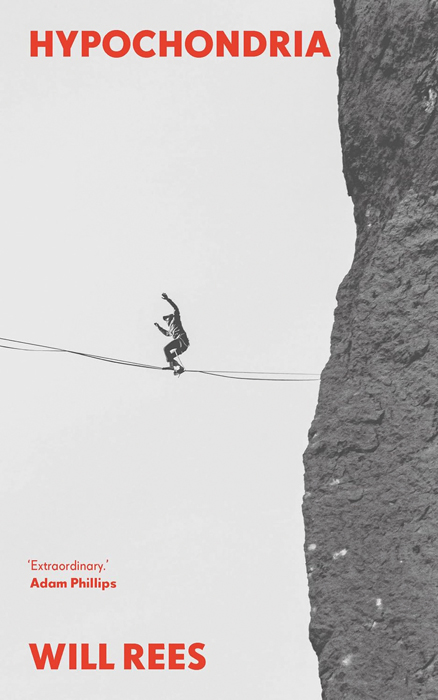
For about a decade I was convinced I was mortally ill. The identity of my illness changed several times, but the fear was always the same: in short, that I was dying; that I had some dreadful and no doubt painful disease that, for all my worrying, I had carelessly allowed to reach the point at which it had become incurable.
My researches required me to seek the help of doctors. Above all, I wanted a scan that would reveal what was the matter with me. But my doctors tended to take a different view – and the greater my fear at their inaction, the more I convinced them that my symptoms were the result of anxiety.
The history of hypochondria is probably as old as humanity itself, but – like so much else – the word itself emerged in Ancient Greece. It comes from hypo, meaning below, and chondrium, referring to the cartilage of the ribs. For around two millennia hypochondria was considered to be a physical disease, seated in the abdomen. It was caused by an excess of black bile and was therefore categorised as a form of melancholy, that ambiguous sickness of body and soul.
Get the latest news and insight into how the Big Issue magazine is made by signing up for the Inside Big Issue newsletter
In his vast tract The Anatomy of Melancholy (1621), Robert Burton wrote that, in addition to gastrointestinal symptoms, hypochondria could cause “fear and sorrow”. In the 18th century – after the anatomists who were now dissecting corpses found no trace of this black bile – hypochondria was redescribed as a nervous illness. It was often considered to be a peculiarly male disease: a counterpart to the hysteria that was said to affect women.
By the Victorian era, long before my friends started calling me a hypochondriac, the concept had settled into its current meaning: a fear of illness so extreme that it becomes a form of illness. That “strangest spectre”, Charlotte Brontë once called it, speaking to a condition that is both airy and incessant.